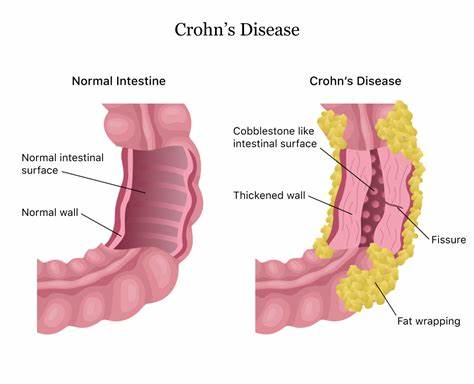
Crohn’s disease is a chronic inflammatory bowel disease that affects the lining of the digestive tract. It is an autoimmune disorder, which means that the body’s immune system mistakenly attacks and damages healthy tissues in the digestive tract. In Crohn’s disease, the immune system mistakenly recognizes harmless substances, such as food particles or gut bacteria, as threats and launches an inflammatory response. This chronic inflammation thickens the intestinal wall, which can cause various complications, including strictures, fistulas, and abscesses. The inflammatory response can also impair the absorption of nutrients, leading to malnutrition and vitamin deficiencies. Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, but it most commonly affects the end of the small intestine (ileum) and the beginning of the colon. The inflammation can occur in patches, with healthy areas of the digestive tract between the affected regions.
MUST READ;6 Tips for Creating a Work-Life Balance
Several types of Crohn’s disease are classified according to the location and extent of inflammation in the digestive tract. Ileocolonic Crohn’s disease is the most common type, affecting the end of the small intestine (ileum) and the beginning of the colon (colon). Ileitis involves inflammation confined to the ileum, which is the final section of the small intestine. Gastroduodenal Crohn’s disease involves inflammation in the stomach and the first part of the small intestine (duodenum). Jejunoileitis affects the upper part of the small intestine (jejunum) and the ileum. Crohn’s colitis is limited to inflammation in the colon (large intestine). Perianal Crohn’s disease involves inflammation around the anus, leading to complications such as fistulas, abscesses, and ulcers. The location and extent of inflammation can influence the symptoms and complications experienced by an individual with Crohn’s disease. It’s important to note that the type of Crohn’s disease can change over time, and the inflammation may spread to other parts of the digestive tract as the disease progresses.
The exact cause of Crohn’s disease is unknown, but it is believed to result from a combination of genetic and environmental factors that trigger an abnormal immune response in the digestive tract. Genetic factors play a role, with certain gene mutations, such as those involving the NOD2 gene, increasing the risk of developing Crohn’s disease. Environmental factors like smoking, a diet high in fat and processed foods, exposure to certain bacteria or viruses, and high levels of stress are potential triggers. These factors are thought to interact with the individual’s genetic predisposition, leading to an inappropriate activation of the immune system. The activated immune cells then attack the healthy cells and tissues in the digestive tract, causing chronic inflammation and the symptoms associated with Crohn’s disease. While the exact mechanisms are not fully understood, it is clear that both genetic and environmental influences contribute to the development and progression of this complex autoimmune disorder.
The main symptoms of Crohn’s disease can vary in severity and may come and go in periods of remission and flare-ups. Common symptoms include abdominal pain, often localized around the navel or lower right abdomen, as well as diarrhea that may be bloody. Patients frequently experience fatigue, weight loss, and fever due to the inflammation and malabsorption of nutrients. Other possible symptoms include loss of appetite, mouth sores, joint pain, and skin rashes like erythema nodosum. Depending on the location and extent of inflammation, some individuals may suffer from nausea, vomiting, or loss of appetite if the disease affects the upper digestive tract. Complications like intestinal strictures (narrowing), fistulas (abnormal connections to other organs or the skin), and malnutrition can also lead to additional symptoms. The severity and combination of symptoms can vary greatly from one person to another, underscoring the highly individualized nature of Crohn’s disease.
Treatment for Crohn’s disease aims to reduce inflammation, induce and maintain remission, and prevent complications while improving the patient’s quality of life. The specific treatment plan is tailored to the individual’s condition, disease severity, and response to medications. Medications commonly used include aminosalicylates (5-ASA drugs) to reduce inflammation, corticosteroids for short-term relief during flare-ups, immunomodulators (like azathioprine or methotrexate) to suppress the immune system, and biological therapies (such as anti-TNF agents or integrin inhibitors) that target specific proteins involved in inflammation. Dietary modifications, such as a low-fiber, low-residue diet, may be recommended during flare-ups or to manage malnutrition. Nutritional support and supplements are often necessary to correct deficiencies. In severe cases or when complications arise, surgery may be required to remove damaged portions of the digestive tract, drain abscesses, or treat strictures or fistulas.
In conclusion, Crohn’s disease is a chronic and complex condition that requires ongoing management and close monitoring by healthcare professionals. While there is currently no cure, early diagnosis and proper treatment can help control the disease, reduce inflammation, alleviate symptoms, and prevent further complications.