Sickle cell disease (SCD), a devastating hereditary illness that affects red blood cells, has long been a problem for both patients and healthcare practitioners. However, in a historic decision, the National Health Service (NHS) in England has approved exagamglogene autotemcel (exa-cel), a ground breaking gene-editing therapy that gives hope to thousands of patients. This approval represents a big step forward in the fight against sickle cell disease because it brings a potential functional cure for the disorder.
MUST READ; The Unsettling Pause on HIV Relief: What It Means for Global Health
What is sickle cell disease?
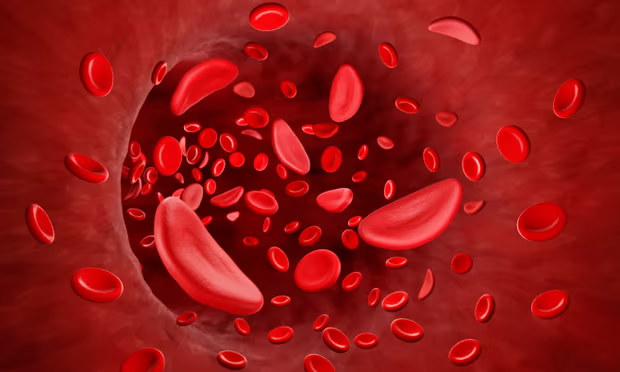
Sickle cell disease is an inherited blood illness that damages haemoglobin, the protein responsible for oxygen transport in the bloodstream. Patients with this disorder have red blood cells that are stiff and shaped like a crescent or “sickle,” rather than the typical round shape. These malformed cells can clump together, obstructing blood flow and causing extreme pain, organ damage, and problems like strokes and infections. SCD predominantly affects people of African, Caribbean, Middle Eastern, and South Asian heritage. It is a lifelong illness that frequently necessitates continuing medical interventions, such as blood transfusions and pain relief.
What Makes Exacel a Game Changer?
Exa-cel is a gene-editing therapy that employs CRISPR technology to fix the defective gene that causes sickle cell disease. Unlike standard treatments, which simply cure symptoms, exa-cel provides a one-time treatment that treats the underlying source of the condition.
How Does Exacel Work?
Blood Stem Cell Extraction: Doctors remove a patient’s blood stem cells.
Gene Editing – The CRISPR-Cas9 gene-editing technique is used to modify the DNA in removed cells, allowing for the synthesis of healthy haemoglobin. Reintroduction into the Body – The changed cells are then reinfused into the patient, causing the body to create normal-shaped red blood cells. Restored Blood Function – Over time, the therapy greatly reduces or eliminates sickle cell problems.
Clinical Trial Success: A Functional Cure
The NHS approved exa-cel based on innovative clinical research that showed extraordinary results: 96.6% of trial participants reported a functional cure, which means they were free of severe pain crises. Patients continued to manufacture healthy red blood cells more than a year after receiving the medication, demonstrating its long-term effectiveness. Many patients no longer needed regular blood transfusions or hospitalizations for problems. This success rate is unique in the history of sickle cell therapy, making exa-cel one of the most significant medical advances of the last few years.
Who is eligible for Exacel?
The NHS permission now applies to patients aged 12 and up who have undergone frequent and severe sickle cell crises. The therapy will be provided at specialized treatment centres in London, Manchester, and Birmingham, ensuring that all qualified patients receive thorough care.
Challenges and Future Implications:
While exa-cel provides tremendous hope, it also comes with challenges:
- Cost: Gene treatments are expensive, and their affordability and accessibility in low-income nations are still an issue.
- Availability: The therapy necessitates highly specialized treatment facilities, which may prevent rapid widespread accessibility.
- Long-term Monitoring: Because gene therapy is relatively new, patients will require long-term follow-ups to assure its sustained efficacy and safety.
Despite these obstacles, exa-cel represents a significant step forward. The NHS’s decision to allow this therapy ushers in a new era of genetic medicine, potentially paving the path for similar therapies for other blood disorders.
In conclusion, for decades, sickle cell patients have had few treatment choices, sometimes experiencing lifelong agony and problems. The NHS’s approval of exagamglogene autotemcel (exa-cel) is a beacon of hope, indicating that sickle cell disease will no longer be a life-threatening condition. As more patients receive access to this new medicine, the world gets closer to a functional cure for sickle cell disease, which will improve the quality of life for thousands.