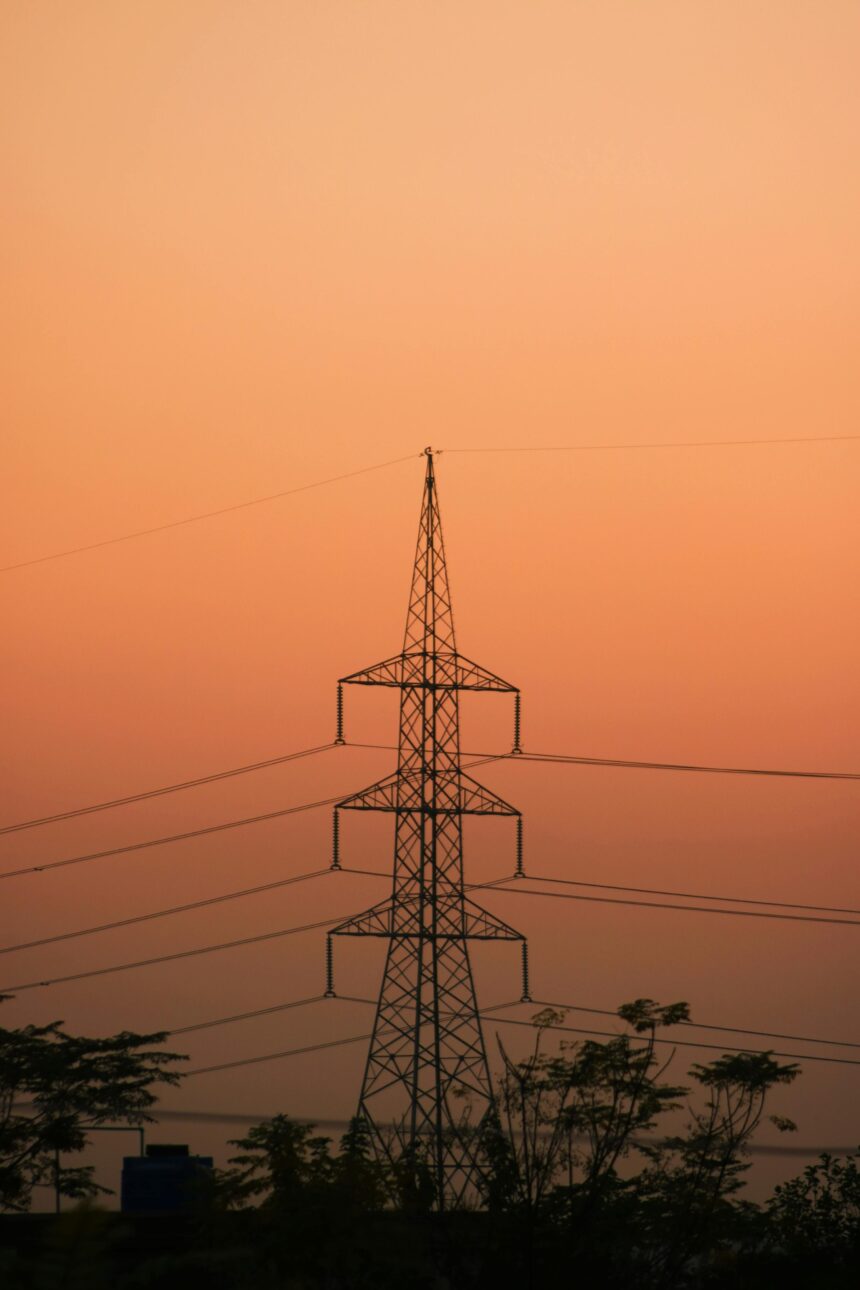
In recent years, Nigeria has experienced periodic power outages, with the national grid frequently collapsing. This issue has far-reaching implications for several areas, including healthcare. The healthcare system significantly relies on a consistent electrical supply to work properly, and with power outages, many hospitals, clinics, and even pharmacies struggle to provide critical services. Here’s a closer look at how Nigeria’s national grid failure directly impacts health, and how these concerns spread to other countries of Africa dealing with similar issues.
MUST READ; Battling the Heatwave in Nigeria: Health Tips and Environmental Impact
Power Dependency in Healthcare Facilities
Hospitals and clinics require electricity to power medical equipment used for diagnosing and treating patients. Ventilators, dialysis equipment, and even simple tools such as X-ray machines and diagnostic scanners require a steady power supply. When the national grid fails, healthcare providers frequently rely on expensive generators as a backup, which are not always reliable or sustainable, particularly during protracted outages. Long-term power outages can cause service delays and possibly jeopardize patient outcomes in rural hospitals and clinics, where resources are already scarce.
Cold Chain Interruptions and Medication Safety
A dependable power supply is essential for sustaining the “cold chain” – the refrigeration needed to store vaccinations, insulin, blood, and other temperature-sensitive pharmaceuticals. Breaks in the cold chain caused by power outages jeopardize the efficacy of these life-saving medicines, particularly vaccinations for diseases such as measles, polio, and tuberculosis, which are included in mandatory immunization programs. Inconsistent storage conditions can cause deterioration and decreased effectiveness, jeopardizing public health initiatives and raising the risk of preventable disease outbreaks.
Increased costs and restricted access to care
Healthcare facilities’ operational costs rise as a result of frequent power outages, which force them to use diesel generators. These rising expenses may result in increasing medical service fees, limiting access to affordable care, particularly in low-income populations. High healthcare expenditures may delay treatment, allowing untreated illnesses to progress. In locations with inadequate healthcare access, this can mean the difference between life and death for people who require rapid care.
Health Risks of Poor Air Quality
Using diesel generators as an alternative to grid electricity adds to air pollution. Diesel emissions emit dangerous particulate matter and contaminants, which can exacerbate respiratory disorders, particularly in densely populated urban areas with a concentration of healthcare services. This pollution can lead to a rise in asthma, chronic bronchitis, and other respiratory difficulties, putting additional strain on the healthcare system for conditions that could be avoided with cleaner and more reliable energy sources.
Broader Implications for Public Health Initiatives
Unreliable power has an impact on not only individual health but also the overall scope of public health programs. Data storage and reporting systems for disease tracking, patient records, and research require consistent electricity. Outages can cause disruptions in these systems, making it difficult to monitor public health trends and respond to outbreaks quickly. For example, during public health catastrophes such as the COVID-19 pandemic, data accuracy, and timeliness are important for successful response, which is made more difficult by frequent power outages.
Solutions and Way Forward
The issues confronting Nigeria’s electrical infrastructure necessitate immediate adjustments, not only for economic growth but also for public health security. Investing in alternative energy sources for healthcare institutions, such as solar power and battery storage, can provide more stable, long-term electricity while reducing reliance on the national grid. Furthermore, prioritizing power infrastructure in rural areas with limited healthcare access helps ensure that even remote clinics have the electricity needed to provide consistent care.
Conclusion; Nigeria’s national grid troubles are more than just a nuisance; they constitute a major public health risk that necessitates both urgent and long-term solutions. Reliable energy is a foundation of good healthcare, and ensuring consistent power is critical to the well-being of all Nigerians. Addressing this issue through sustainable and decentralized energy solutions could provide the healthcare sector a much-needed boost, helping communities throughout Nigeria and beyond.